|
History & Borrelia Species
* Brief History of Lyme Disease
* Borrelia Species by Continent * Other Borrelia Spirochetes & Diseases |
Lyme Borreliosis : Brief History
Investigations first began into Lyme disease (LD) in the USA in 1975 after two concerned mothers, Polly Murray and Judith Mensch from Old Lyme in Connecticut contacted the health department about their sick children and what they felt was an abnormally high number of children with “juvenile rheumatoid arthritis” in their area. One of the scientists involved in the research of the cluster of patients in Connecticut, Willy Burgdorferi, identified the bacteria responsible for Lyme disease as a spirochete belonging to the borrelia genre in 1981 (Two dates 1981/1982 seem to be used interchangeably in various literature: 1981 is the year the ‘discovery’ was made, whilst 1982 is the publishing date of the journal article in which the finding is described). As such this first species was named Borrelia burgdorferi, and being the first species identified, it is typically known as B burgdorferi sensu stricto (in the strictest sense).
Due to the original beginnings/investigation, LD was initially presumed to be a primarily arthritic condition, however it was soon found to have dermatological and neurological manifestations. In Europe, clinical aspects of LD have been written about in medical journals since the 1800’s. A skin condition which is now associated with chronic LD, acrodermatitis chronic atrophicans (ACA), was noted in patients of a German doctor, Alfred Buchwald in 1883, whilst the rash that some LD patients observe, known as erythema migrans (EM) was originally described in 1910 by a Swedish dermatologist, Arvid Afzelius as erythema chronicum migrans (ECM). In 1922, French physicians, Garin and Bujadoux, described neurological (Meningopolyneuritis) symptoms which occurred in a patient after an Ixodes hexagonus tick bite.
In the thirty years since the original investigations began, numerous other species of borrelia have been identified and along with B burgdorferi sensu stricto, are collectively classified as belonging to the Borrelia burgdorferi sensu lato complex. Whilst all the species in the sensu lato complex may be classified as belonging to the Lyme borreliosis group (1,2), another group of borrelia, B. miyamotoi, has recently been reported to cause relapsing fever and Lyme disease-like symptoms in humans (2,3). B. miyamotoi was first described in Japan in 1995 as a new species of borrelia (4) that resemble relapsing fever species in some ways and Lyme borreliosis species in others” (5: Pg 1129) . Spirochetes that were found to be closely related to B. miyamotoi (B. miyamotoi sensu lato) have been reported in a number of studies in the United States from 2001 (eg: 6-8) and Europe since 2002 (9). Genetic sequencing of B. miyamotoi has revealed that it is closely related to the B. lonestari species of borrelia (1). B. lonestari is associated with a “Lyme-like” disease known as, Southern Tick Associated Rash Illness (STARI), or Masters disease, which is reportable to the Centre for Disease Control (CDC) as Lyme disease (10).
Due to the original beginnings/investigation, LD was initially presumed to be a primarily arthritic condition, however it was soon found to have dermatological and neurological manifestations. In Europe, clinical aspects of LD have been written about in medical journals since the 1800’s. A skin condition which is now associated with chronic LD, acrodermatitis chronic atrophicans (ACA), was noted in patients of a German doctor, Alfred Buchwald in 1883, whilst the rash that some LD patients observe, known as erythema migrans (EM) was originally described in 1910 by a Swedish dermatologist, Arvid Afzelius as erythema chronicum migrans (ECM). In 1922, French physicians, Garin and Bujadoux, described neurological (Meningopolyneuritis) symptoms which occurred in a patient after an Ixodes hexagonus tick bite.
In the thirty years since the original investigations began, numerous other species of borrelia have been identified and along with B burgdorferi sensu stricto, are collectively classified as belonging to the Borrelia burgdorferi sensu lato complex. Whilst all the species in the sensu lato complex may be classified as belonging to the Lyme borreliosis group (1,2), another group of borrelia, B. miyamotoi, has recently been reported to cause relapsing fever and Lyme disease-like symptoms in humans (2,3). B. miyamotoi was first described in Japan in 1995 as a new species of borrelia (4) that resemble relapsing fever species in some ways and Lyme borreliosis species in others” (5: Pg 1129) . Spirochetes that were found to be closely related to B. miyamotoi (B. miyamotoi sensu lato) have been reported in a number of studies in the United States from 2001 (eg: 6-8) and Europe since 2002 (9). Genetic sequencing of B. miyamotoi has revealed that it is closely related to the B. lonestari species of borrelia (1). B. lonestari is associated with a “Lyme-like” disease known as, Southern Tick Associated Rash Illness (STARI), or Masters disease, which is reportable to the Centre for Disease Control (CDC) as Lyme disease (10).
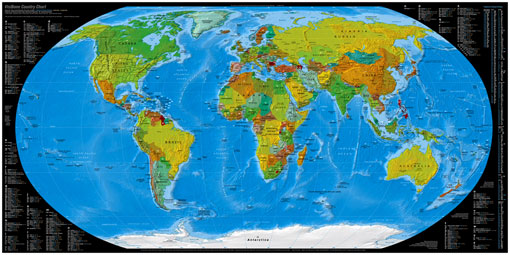
Worldwide there has been over 20 borrelia species identified as being associated to Lyme, or Lyme-like disease in humans.
Borrelia Species by Continent
Borrelia Species associated to Lyme Disease / Borreliosis in Humans identified in various continents include:
(Please remember this is not a full list and does not cover a number of countries/ other species isolated)
North America: B. burgdorferi ss*, B. americana, B. andersonii, B. bissettii*, B. californiensis, B. carolinensis, B. garinii*,
B. kurtenbachii. B. miyamotoi sl** and B. lonestari***
Canada: B. burgdorferi ss*, B. bissettii*, BC genotypes (3 distinct though as yet unnamed species)
Europe: B. burgdorferi ss*, B. afzelii*, B. bavariensis* (previously known as B. garinii OspA serotype 4), B. bissettii*,
B. garinii*, B. finlandensis, B. lusitaniae*, B. spielmanii*, B. valaisiana* and B. miyamotoi sl**
Asia: B. afzelii*, B. garinii*, B. lusitaniae*, B. sinica, B. valaisiana* , B. yangtze and B. miyamotoi**
The first isolation of B. burgdorferi ss* in Southern China was from a hare in 2011, with further research required to confirm the spread into Asia (11).
Japan: B. garinii*, B. japonica, B. tanukii, B. turdi, B. valaisiana* and B. miyamotoi**
(Please note: Whilst it is acknowledged that Japan is a part of the Asian continent; the studies examining the incidence of Lyme disease usually differentiate between Asia and Japan as it is a “stand-alone” island).
Australia: B. queenslandica
*Known to be pathogenic **Relapsing Fever/ Lyme-like disease ***Lyme-like illness
Whilst all the above species have been isolated and identified from ticks and animals (and therefore can potentially cause disease in humans), it is not until a species has been isolated from human tissue, that it is acknowledged as pathogenic.
(See references 12-16 for senso lato species and pathogenicity).
The ability to understand the pathogenicity of each species and the development of adequate diagnostic/ testing procedures to ascertain human infection status is made that much more difficult by the fact that within the above mentioned species there are 100’s of strain variations (eg:17-24) involved. For example, until recently B. bavariensis was known as B. garinii OspA serotype 4. Sequence analysis and testing revealed that this strain (serotype 4) was specific to rodent hosts (and unable to survive bird serum), with the opposite being shown for B. garinii serotypes 3,5,6 and 7, which are bird associated strains, and unable to survive in rodent serum. Due to the sequence analysis and host differences, B. garinii OspA serotype 4 was therefore classified as a separate species, B. bavariensis (17). Another quick example is that vector differences, as well as sequence analysis, reveals that the B. garinii and B. valaisiana strains from Europe differ from the B. garinii and B. valaisiana-related strains from Asia (18,19).
These above brief examples outline why it is “important to develop alternative identification tools which are able to distinguish Borrelia strains not only at the specific level but also at the intraspecific level” (25: Pg 509). Understanding that there is such an enormous number of strain diversities, even within species of borrelia, allows for a better appreciation as to why Lyme disease is primarily a clinical diagnosis. When testing for borrelia infection, it is imperative that there is an understanding that the accuracy of the tests are limited by various factors, one of which is the species diversity, and that for more accurate testing and diagnosis, “the choice of a B. burgdorferi sensu lato strain for an antigen in serological testing is important” (26: Pg 52).
(Please remember this is not a full list and does not cover a number of countries/ other species isolated)
North America: B. burgdorferi ss*, B. americana, B. andersonii, B. bissettii*, B. californiensis, B. carolinensis, B. garinii*,
B. kurtenbachii. B. miyamotoi sl** and B. lonestari***
Canada: B. burgdorferi ss*, B. bissettii*, BC genotypes (3 distinct though as yet unnamed species)
Europe: B. burgdorferi ss*, B. afzelii*, B. bavariensis* (previously known as B. garinii OspA serotype 4), B. bissettii*,
B. garinii*, B. finlandensis, B. lusitaniae*, B. spielmanii*, B. valaisiana* and B. miyamotoi sl**
Asia: B. afzelii*, B. garinii*, B. lusitaniae*, B. sinica, B. valaisiana* , B. yangtze and B. miyamotoi**
The first isolation of B. burgdorferi ss* in Southern China was from a hare in 2011, with further research required to confirm the spread into Asia (11).
Japan: B. garinii*, B. japonica, B. tanukii, B. turdi, B. valaisiana* and B. miyamotoi**
(Please note: Whilst it is acknowledged that Japan is a part of the Asian continent; the studies examining the incidence of Lyme disease usually differentiate between Asia and Japan as it is a “stand-alone” island).
Australia: B. queenslandica
*Known to be pathogenic **Relapsing Fever/ Lyme-like disease ***Lyme-like illness
Whilst all the above species have been isolated and identified from ticks and animals (and therefore can potentially cause disease in humans), it is not until a species has been isolated from human tissue, that it is acknowledged as pathogenic.
(See references 12-16 for senso lato species and pathogenicity).
The ability to understand the pathogenicity of each species and the development of adequate diagnostic/ testing procedures to ascertain human infection status is made that much more difficult by the fact that within the above mentioned species there are 100’s of strain variations (eg:17-24) involved. For example, until recently B. bavariensis was known as B. garinii OspA serotype 4. Sequence analysis and testing revealed that this strain (serotype 4) was specific to rodent hosts (and unable to survive bird serum), with the opposite being shown for B. garinii serotypes 3,5,6 and 7, which are bird associated strains, and unable to survive in rodent serum. Due to the sequence analysis and host differences, B. garinii OspA serotype 4 was therefore classified as a separate species, B. bavariensis (17). Another quick example is that vector differences, as well as sequence analysis, reveals that the B. garinii and B. valaisiana strains from Europe differ from the B. garinii and B. valaisiana-related strains from Asia (18,19).
These above brief examples outline why it is “important to develop alternative identification tools which are able to distinguish Borrelia strains not only at the specific level but also at the intraspecific level” (25: Pg 509). Understanding that there is such an enormous number of strain diversities, even within species of borrelia, allows for a better appreciation as to why Lyme disease is primarily a clinical diagnosis. When testing for borrelia infection, it is imperative that there is an understanding that the accuracy of the tests are limited by various factors, one of which is the species diversity, and that for more accurate testing and diagnosis, “the choice of a B. burgdorferi sensu lato strain for an antigen in serological testing is important” (26: Pg 52).
Other Borrelia Spirochetes and Diseases
Unless specifically stated otherwise, the term borrelia (ie: borrelia was found in a certain host) on this website is used in reference to borrelia spirochetes responsible for Lyme disease/borreliosis in humans.
This note is made as spirochetes of the borrelia family are also responsible for other known diseases in humans and animals. Some of these include:
Relapsing Fever in humans - eg: B. duttonii, B. hermsii, B. turicatae and B. recurrentis
(B. recurrentis, is transmitted by the human body louse, and is the only species acknowledged as being transmitted via an insect rather than a tick).
Spirochetosis in birds - eg: B. anserina
(Borrelia species such as B. garinni and B. valaisiania responsible for Lyme disease in humans is also carried in birds).
Bovine borreliosis - eg: B. theilerii and B. coriaceae
(As well as being able to cause disease in humans, both the B. burgdorferi and B. garinii species have also been found associated with borreliosis in cattle).
Borrelia responsible for the above diseases are differentiated from the borrelia species that are responsible for Lyme disease/borreliosis in humans, by genetic and vector (different tick species) differences. Although it should be noted that differentiating via tick species that transmit the disease is starting to become more ambiguous with species such as B. miyamoto, in which the vectors differ from the typical pattern. Typically, spirochetes responsible for Lyme disease are transmitted via hard ticks, whist relapsing fever is transmitted via soft ticks, however with the Miyamoto species, both hard and soft ticks have been found capable of transmitting the disease, and also unlike other borrelia species responsible for Lyme disease, the bacteria is passed from the female tick to the egg/larvae (eg 1,5,6). \
Relapsing Fever in humans - eg: B. duttonii, B. hermsii, B. turicatae and B. recurrentis
(B. recurrentis, is transmitted by the human body louse, and is the only species acknowledged as being transmitted via an insect rather than a tick).
Spirochetosis in birds - eg: B. anserina
(Borrelia species such as B. garinni and B. valaisiania responsible for Lyme disease in humans is also carried in birds).
Bovine borreliosis - eg: B. theilerii and B. coriaceae
(As well as being able to cause disease in humans, both the B. burgdorferi and B. garinii species have also been found associated with borreliosis in cattle).
Borrelia responsible for the above diseases are differentiated from the borrelia species that are responsible for Lyme disease/borreliosis in humans, by genetic and vector (different tick species) differences. Although it should be noted that differentiating via tick species that transmit the disease is starting to become more ambiguous with species such as B. miyamoto, in which the vectors differ from the typical pattern. Typically, spirochetes responsible for Lyme disease are transmitted via hard ticks, whist relapsing fever is transmitted via soft ticks, however with the Miyamoto species, both hard and soft ticks have been found capable of transmitting the disease, and also unlike other borrelia species responsible for Lyme disease, the bacteria is passed from the female tick to the egg/larvae (eg 1,5,6). \
© Karen Smith, B. Psych (Hons), 2012 -2015